Amyotrophic lateral sclerosis (a-my-o-TROE-fik LAT-ur-ul skluh-ROE-sis), or ALS, is a group of rare neurological diseases that mainly involve the nerve cells (neurons) responsible for controlling voluntary muscle movement.
A-myo-trophic comes from the Greek language. “A” means no or negative. “Myo” refers to muscle, and “Trophic” means nourishment—“No muscle nourishment.” When a muscle has no nourishment, it “atrophies” or wastes away. “Lateral” identifies the areas in a person’s spinal cord where portions of the nerve cells that signal and control the muscles are located. As this area degenerates it leads to scarring or hardening (“sclerosis”) in this region of the cord.
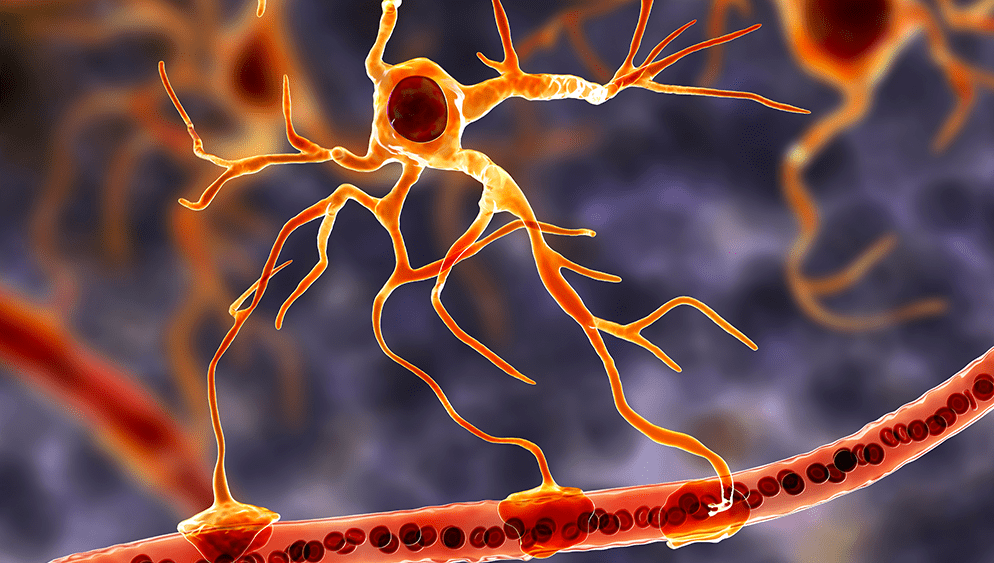
ALS belongs to a wider group of disorders known as motor neuron diseases, which are caused by gradual deterioration (degeneration) and death of motor neurons. Motor neurons are nerve cells that extend from the brain to the spinal cord and to muscles throughout the body. These motor neurons initiate and provide vital communication links between the brain and the voluntary muscles.
Messages from motor neurons in the brain (called upper motor neurons) are transmitted to motor neurons in the spinal cord and to motor nuclei of brain (called lower motor neurons) and from the spinal cord and motor nuclei of brain to a particular muscle or muscles.
In ALS, both the upper motor neurons and the lower motor neurons degenerate or die, and stop sending messages to the muscles. Unable to function, the muscles gradually weaken, start to twitch (called fasciculations), and waste away (atrophy). Eventually, the brain loses its ability to initiate and control voluntary movements.
Early symptoms of ALS usually include muscle weakness or stiffness in a limb. Gradually all muscles under voluntary control are affected, and individuals lose their strength and the ability to speak, eat, move, and even breathe.
ALS is often called Lou Gehrig’s disease, after first baseman Lou Gehrig from the Yankees who developed symptoms in 1939.
Mr. Gehrig retired from baseball and gave his famous speech on July 4, 1939, when he called himself the ‘luckiest man’.
ALS is inherited in 5% to 10% of people. For the rest, the cause isn’t known.
Researchers continue to study possible causes of ALS. Most theories center on a complex interaction between genetic and environmental factors.
Established risk factors for ALS include:
• Heredity. Five to 10 percent of the people with ALS inherited it (familial ALS). In most people with familial ALS, their children have a 50-50 chance of developing the disease.
• Age. ALS risk increases with age, and is most common between the ages of 40 and the mid-60s.
• Sex. Before the age of 65, slightly more men than women develop ALS. This sex difference disappears after age 70.
• Race and ethnicity. Most likely to develop the disease are Caucasians and non-Hispanics.
Environmental factors, such as the following, might trigger ALS.
• Smoking. Smoking is the only likely environmental risk factor for ALS. The risk seems to be greatest for women, particularly after menopause.
• Environmental toxin exposure. Some evidence suggests that exposure to lead or other substances in the workplace or at home might be linked to ALS. Much study has been done, but no single agent or chemical has been consistently associated with ALS.
• Military service. Studies indicate that people who have served in the military are at higher risk of ALS. It’s unclear what about military service might trigger the development of ALS. It might include exposure to certain metals or chemicals, traumatic injuries, viral infections, and intense exertion.
Genetics
An important step toward determining ALS risk factors was made in 1993 when scientists supported by the National Institute of Neurological Disorders and Stroke (NINDS) discovered that mutations in the SOD1 gene were associated with some cases of familial ALS. Although it is still not clear how mutations in the SOD1 gene lead to motor neuron degeneration, there is increasing evidence that the gene playing a role in producing mutant SOD1 protein can become toxic.
Since then, more than a dozen additional genetic mutations have been identified, many through NINDS-supported research, and each of these gene discoveries is providing new insights into possible mechanisms of ALS.
The discovery of certain genetic mutations involved in ALS suggests that changes in the processing of RNA molecules may lead to ALS-related motor neuron degeneration. RNA molecules are one of the major macromolecules in the cell involved in directing the synthesis of specific proteins as well as gene regulation and activity.
Other gene mutations indicate defects in the natural process in which malfunctioning proteins are broken down and used to build new ones, known as protein recycling. Still others point to possible defects in the structure and shape of motor neurons, as well as increased susceptibility to environmental toxins. Overall, it is becoming increasingly clear that a number of cellular defects can lead to motor neuron degeneration in ALS.
In 2011 another important discovery was made when scientists found that a defect in the C9ORF72 gene is not only present in a significant subset of individuals with ALS but also in some people with a type of frontotemporal dementia (FTD). This observation provides evidence for genetic ties between these two neurodegenerative disorders. Most researchers now believe ALS and some forms of FTD are related disorders.
As the disease progresses, ALS causes complications, such as:
Breathing problems
Over time, ALS paralyzes the muscles you use to breathe. You might need a device to help you breathe at night, similar to what someone with sleep apnea might wear. For example, you may be given continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) to assist with your breathing at night.
Some people with advanced ALS choose to have a tracheostomy — a surgically created hole at the front of the neck leading to the windpipe (trachea) — for full-time use of a respirator that inflates and deflates their lungs.
The most common cause of death for people with ALS is respiratory failure. On average, death occurs within three to five years after symptoms begin. However, some people with ALS live 10 or more years.
Speaking problems
Most people with ALS develop trouble speaking. This usually starts as occasional, mild slurring of words, but becomes more severe. Speech eventually becomes difficult for others to understand, and people with ALS often rely on other communication technologies to communicate.
Eating problems
People with ALS can develop malnutrition and dehydration from damage to the muscles that control swallowing. They are also at higher risk of getting food, liquids or saliva into the lungs, which can cause pneumonia. A feeding tube can reduce these risks and ensure proper hydration and nutrition.
Dementia
Some people with ALS have problems with memory and decision-making, and some are eventually diagnosed with a form of dementia called frontotemporal dementia.
Most people with ALS die from respiratory failure, usually within 3 to 5 years from when the symptoms first appear. However, about 10 percent of people with ALS survive for 10 or more years.